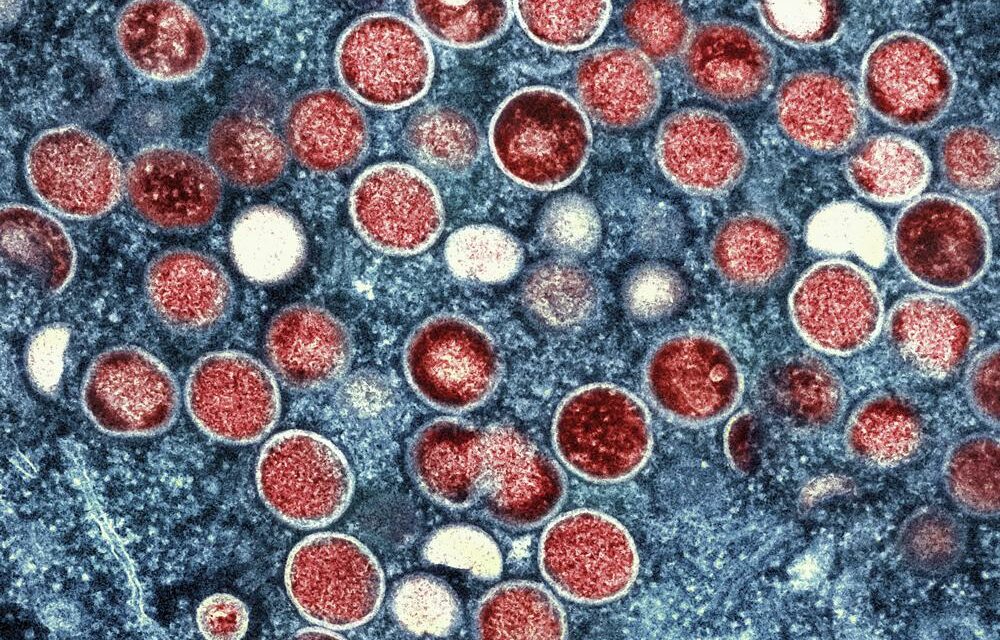
With the United States declaring monkeypox as the latest national public health emergency, Duke University held a panel to share what people ought to know – both about limiting transmission and busting stigmas around the illness.
The predominant symptom of the virus is a rash on the hands, mouth or genital region that blisters and scabs before healing. Fever, swollen lymph nodes and exhaustion are also common symptoms. Monkeypox is known for its ability to spread through prolonged skin-to-skin contact and for sometimes taking three weeks to display symptoms.
Dr. Cameron Wolfe is an infectious disease specialist for Duke Health. He said while the virus has been endemic in parts of western and central Africa, it has been common to see cases reach the U.S. before. Beyond an outbreak of a few dozen people in the early 2000’s, however, monkeypox never had a true foothold in the country until now.
Wolfe said while early perceptions may be the illness mostly spreads between men having sex with men, this outbreak far more indiscriminate.
“We’ve seen,” he said, “that intimate contact mainly so far occurs through sexual networks, partner networks, friendship networks – dominated actually so far by men, particularly men who had male sexual partners.
“But I’d like to also emphasize,” Wolfe added, “early on there’s nothing about the way the virus moves that cares about your agenda, who you love, who you hang out with. There is no reason that this needs to stay in those populations, there’s already been women and kids who’ve been affected as well.”
Dr. Ibukun Kalu, a pediatrician at Duke Health, confirmed there have already been several cases in children. She said while parents’ initial thoughts may be that school or daycare settings present the most risk, it’s actually the home environment where prolonged contact is more common and where the virus has spread.
Kalu also pointed to a tricky element to identifying the illness in child cases.
“The key presenting symptom has been a rash,” she said, “and children get lots of rashes. There are other vaccine-preventable infections that can cause fever and rashes, and this is a great time to ensure your child is up to date with all routine vaccinations. For example, [there are] chicken pox, measles, and other things that we wouldn’t need to test for if we see a child with fever and a rash.”
Despite the variety of cases, Dean of Duke’s School of Nursing Vincent Guilamo-Ramos said messaging around how monkeypox spreads will be critical. He said it’s not only because some people’s trust of health systems eroding, but because it will be key to break any stigmatization around who is catching the virus.
“We need to make sure that we’re not blaming,” said Ramos, “and that we’re actually reaching out to communities – to try to seek partnerships, [to think] about ways that we can work together from a public health model to really try to prevent this, to mitigate, to really reach people who are most at risk and ask them to help us to hold transmission.”
Kalu echoed that messaging is also critical to prevent stigmatizing people who may have pre-existing skin conditions or manifestations. She said with kids, they may not be able to explain all their conditions – so childcare settings should not rush to conclusions.
“Policies around school attendance or daycare attendance should allow room for medical evaluation, but not carte blanche remove kids from those settings with any potential skin inflammation,” said Kalu. “So, those will be the caveats and as we learn more, hopefully we will share more and adjust guidance accordingly.”
A main reason people need to be reached is to promote testing and tracking the spread of the virus, said Wolfe.
“I think the testing is really important here,” he said, “because not only does it help the individual know that they’re positive or not, it also helps us set up contact tracing. Tracing is something that we did at the beginning of COVID-19 that’s really crucial here, because people may not know that they’ve been exposed and we actually have interventions here with vaccines to help exposed people.”
Ramos said he’s pleased there is already guidance out for people experiencing symptoms, as well as safer sex guidelines and information for those who live in shared space with others.
“Particularly if somebody in the home has monkeypox,” he said, “how can be prevented forward transmission within the home? Again, the CDC has put some terrific guidelines on their website to try to think about ways an individual can isolate in the home, and some very practical things that can be done [to] reduce the chances of forward transmission to people within your home.”
For resources and more details about monkeypox response, visit the Centers for Disease Control website.
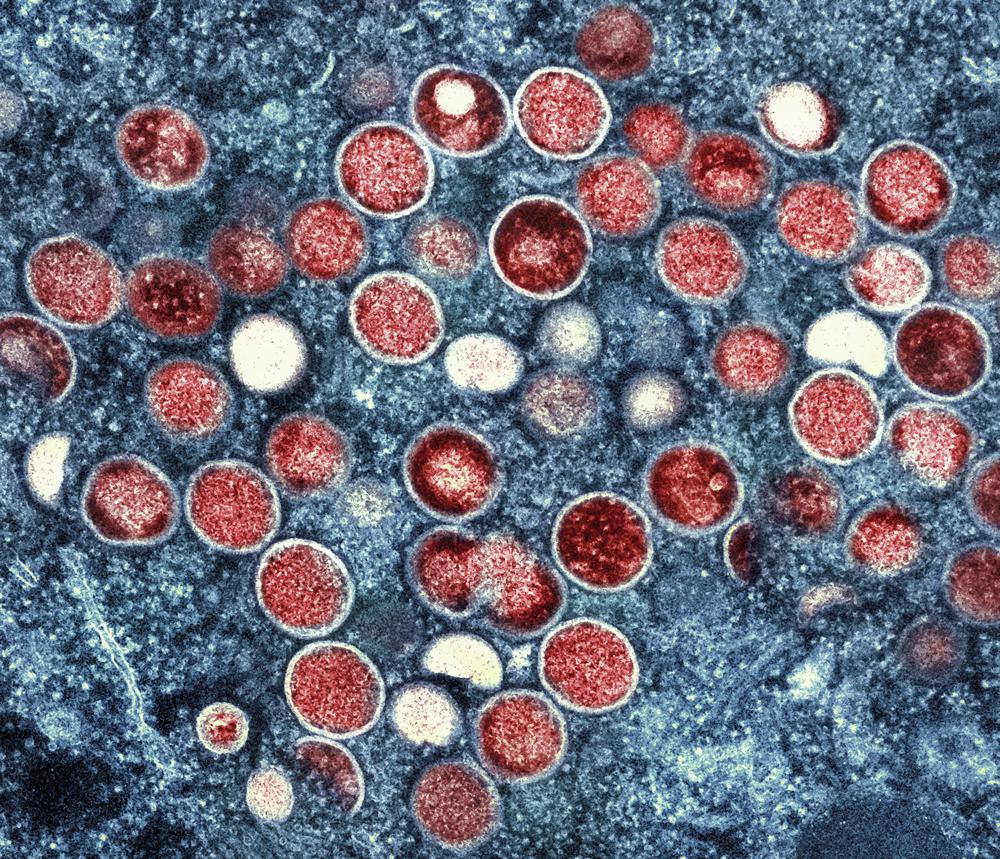
Photo via National Institute of Allergy and Infectious Diseases and Associated Press.
Chapelboro.com does not charge subscription fees, and you can directly support our efforts in local journalism here. Want more of what you see on Chapelboro? Let us bring free local news and community information to you by signing up for our biweekly newsletter.