North Carolina’s health agency on Monday awarded four conventional insurers and one physician partnership the contracts to treat most of the state’s Medicaid patients through managed-care coverage.
The winning contract bidders selected by the state Department of Health and Human Services will care for 1.6 million Medicaid recipients starting late this year or early next year. The contracts are worth about $6 billion annually for up to five years, making them the largest procurement in the department’s history.
AmeriHealth Caritas, WellCare, UnitedHealth Care and Blue Cross and Blue Shield of North Carolina all were awarded statewide contracts. A group called Carolina Complete Health — composed of the North Carolina Medical Society, insurer Centene and the state Community Health Center Association — will receive a contract for two regions of the state.
The awards mark the biggest step to date in shifting Medicaid from traditional fee-for-service coverage to flat monthly allotments to the companies for each patient covered. The amounts have not been finalized.
While these “prepaid health plan” contractors will have to spend most of their payments on medical services and activities, their profits or losses also likely will depend on levels of patient health. They can also face monetary withholdings or penalties for failing to meet standards, state health Secretary Mandy Cohen said.
The managed-care coverage begins in phases, with enrollees in 27 northern counties stretching from Boone to Rocky Mount and including the Triangle and Triad coming on board in November. The other counties will follow in February 2020.
“Our work starts today to build toward that Nov. 1 date,” Cohen told reporters. “The award winners are going to start contracting with doctors and hospitals to build their Medicaid networks.” Recipients also will receive open-enrollment information and will choose an insurer. Those who don’t pick one will be placed in a plan based on their needs and location, Cohen said.
The legislature ordered the Medicaid transition to managed care in a 2015 law, with supporters arguing it would keep Medicaid costs in checks while improving the health of recipients. Lawmakers directed that four statewide contracts be awarded and that up to 12 regional contracts be given to “provider-led entities.” Bids from eight organizations were received.
A department evaluation team recommended the statewide contractors but no regional contractors. But Deputy DHHS Secretary Dave Richard recommended to Cohen that a regional contract be awarded to Carolina Complete Health to seek consistency with the legislation, provide more competition and encourage treatment innovation. Cohen made the final award decisions, which can be appealed.
Carolina Complete Health “still met overall expectations” as set by the evaluation team, Richard wrote Cohen last week. The organization will provide coverage in counties including the cities of Hickory, Charlotte, and Wilmington.
North Carolina’s Medicaid program serves 2 million residents — mostly poor children, older adults and the disabled. The mentally ill, substance abusers and people with developmental disabilities will be phased in over the next several years.
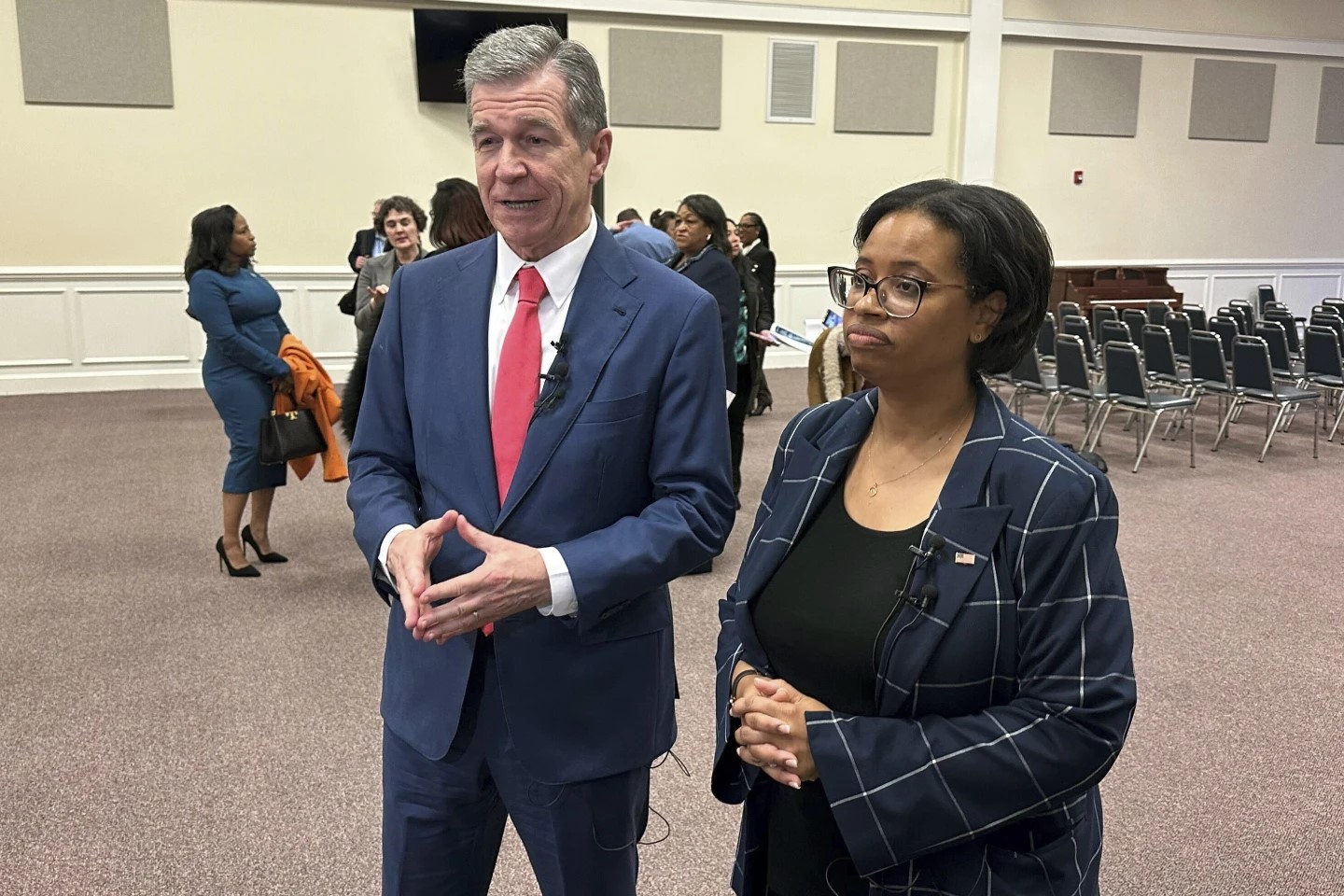
The shift to managed care occurs this year as lawmakers are expected to hold a robust debate over whether North Carolina should expand Medicaid coverage to another 300,000 to 500,000 people in the state through former President Barack Obama’s health care law. Democratic Gov. Roy Cooper and his legislative allies are making it a top priority after eroding Republican majorities in the General Assembly in November.